Abstract
Mantle Cell Lymphoma (MCL) is a difficult to cure, highly heterogeneous, and aggressive form of non-Hodgkin lymphoma comprising roughly 7% of all cases with a high recurrence rate and poor long-term prognosis. The reported progression-free survival is about 1-2 years, and median overall survival/OS <3 years. Current first-line MCL therapies include combination regimens like R-CHOP, R-DHAP, Hyper-CVAD, VcR-CAP, etc. However, although patients respond well to initial treatment, most eventually progress to relapsed disease state. BTKis (Bruton's tyrosine kinase inhibitors) such as Ibrutinib are standard targeted therapeutic options for refractory or relapsed (R/R) MCL. The proteasome inhibitor (PI) drug Bortezomib/Velcade/Bz is another FDA-approved targeted drug for R/R MCL. However, despite these recent advances in the treatment landscape, R/R MCL still remains incurable with limited therapeutic options and a median OS<10-15 months. Therefore, there is an unmet need to discover novel drugs against R/R MCL.
Previously, we have demonstrated that Clofazimine (CLF), an anti-leprosy drug, could potentially be repurposed for the treatment of chronic myeloid leukemia and PI/IMiD resistant multiple myeloma that also targets subclones representing putative stem-like-cells (CSCs). Notably, using single-cell analysis and high dimensional immunophenotyping or CyTOF (Cytometry Time of Flight), we have also identified molecular networks underpinning CLF+PI synergy. We hypothesize that CLF has strong potential to be repurposed as a novel anti-MCL drug, particularly in a relapsed/refractory setting.
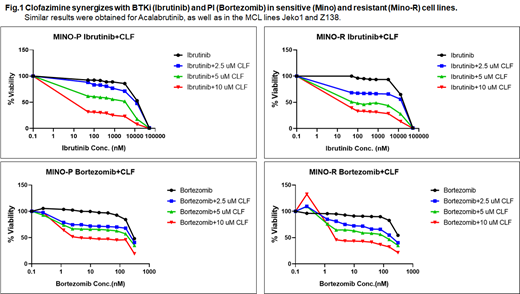
For this purpose, we used MCL cell lines representing drug-sensitive (JEKO1, MINO), innate PI/BTKi-resistance (Z138; representing refractory patients), and clonally-derived acquired PI/BTKi-resistance (MINO-R; representing relapse patients) as in vitro model systems and showed i) the efficacy of CLF as a single agent (IC 50= 6.9±3.6 uM) and ii) in combination with PIs (Bz) and BTKis (Ibrutinib, Acalabrutinib) against innate and acquired resistant MCL (Fig.1), as well as iii) the unique targeting of putative CSCs by CLF. Remarkably, CLF+BTKi/PI combination lowered the effective BTKi and PI doses required to achieve desired therapeutic response by >10-folds (estimated dose reduction index for BTKi and PI were 12.43 and 10.99, respectively). Further, mRNA-sequencing followed by differential gene expression analysis using DESeq2 and EdgeR revealed that the top significantly upregulated genes following PI+CLF treatment were GSR, DAP3, and DOK1, which have reported anti-tumorigenic activity. The top significantly downregulated genes EHD1, CBX8, DDX17, SOX12, and COMMD3 have reported pro-survival function. Ingenuity pathway analysis revealed protein ubiquitination pathway and cell cycle arrest at the G2/M phase as the top canonical pathways. Causal network analysis showed synergistic drug action significantly elevated the levels of oxidative stress and unfolded protein response. Additionally, PI+CLF combination potentiated AMPK mediated down-regulation of the mTOR signaling pathway, which further led to direct reduction of Cyclin D1 (aberrantly expressed in MCL) and the downregulation of eIF4-p70S6K signaling. The synergistic drug activity also led to the downregulation of oncogenic pathways like p38 MAPK and NF-kB signaling.
Recent studies have indicated that intra-tumor heterogeneity due to the presence of stem-like cells in MCL (MCL-CSCs), including CD45+CD19- MCL-initiating cells (MCL-ICs), relatively quiescent-highly clonogenic aldehyde dehydrogenase (ALDH)+ cells and side populations (SP) may drive drug resistance and disease relapse. Notably, we found that several of the differentially regulated genes are critical for the maintenance and functioning of CSCs. For example, PI+CLF combination downregulates Wnt/β catenin signaling, which is found to be frequently overexpressed in MCL-ICs. HIPPO, another signaling pathway involved in the maintenance of cancer stem-ness and emergence of drug resistance, was also down-regulated. Currently, we are validating the specific targeting of putative MCL-CSCs by CLF. Next, we plan to replicate our findings using PDX models of MCL.
CLF is an FDA-approved drug as well as on WHO's List of Essential Medicines. Thus, our study introduces CLF as a novel, safe, and inexpensive therapeutic option for the management of R/R MCL.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal